Do you think understanding neuro is difficult?
Do you think practising neuro rehab is more complicated and tiring?
DO you think it takes long time to show recovery in neurological cases?
Most of the student’s feel that neuro rehab is very difficult to understand because we can’t imagine and understand how neuro Physiology work? How does neuro recovery occurs? How to enhance and fasten neuro rehabilitation process?
Where as musculoskelatle rehab is we can see the changes in the range we can measure the changes in strength and function. But in neuro it is very difficult see and measure the changes. First of all students don’t understand the neuro rehab approaches very, application of these in treatment is far fetched goal.
One day during my master training program, i asked the question to a very famous neurologist from Jahangir Hospital DR. N. R. Ichaporia.

Why neuro rehab is do difficult?
DR. Ichaporia said:
“Neuro rehab is not difficult, It is the way it is been taught makes is more difficult!”
This answer changed my mission of life. i understood that the training has to change. It has to change in such a way that it should become easy and simple for everyone to understand neuro rheab. Based on this incident with Dr. Ichaporia i have made my mission of life as
“Making neuro rehab Simple”….. Gajanan Bhelerao
I have attended multiple workshop and course in neuro rehabilitation to understand it better in order make it simple. After completing multiple course and 15 years of extensive practice in neuro rehab and teaching for 11 years in physiotherapy college about neuro rehab, i have found methods of how to make neuro rehab simple to understand and practice.
Now i want to share my experience and knowledge all the budding therapist who aspire work in neuro rehabilitation. So we formaed a organisation GB School of neuro rehab and Aquatic therapy for training of therapist and treatment of patients with neurological disorders.
With aim of sharing our knowledge and empowering budding therapist we have started
“Neuro rehab Education series 2018”
| DATE | TOPIC | PERIOD | FEES | CAPACITY |
| 17/03/2018 & 18/03/2018 | MOTOR RELEARNING PART 1. MOTOR RELEARNING PROGRAM | 2 DAYS , | RS 5000/- | 25 THERAPIST |
| 15/04/2018 | ATAXIA: MOVEMENT DYSFUNCTION & ITS MANAGEMENT | 1 DAY | RS 3000/- | 25 THERAPIST |
| 05/05/2018 & 06/05/2018 | MOTOR RELEARNING PART 2: ADVANCE UPPER LIMB CONTROL TRAINING | 2 DAYS | RS 6000/- | 25 THERAPIST |
| 26/05/2018 & 27/05/2018 | MOTOR RELEARNING PART 3: ADVANCE LOWER LIMB CONTROL TRAINING | 2 DAYS | RS 6000/- | 25 THERAPIST |
BANKING DETAILS : BHALERAO SCHOOL OF NEURO REHAB PVT LTD
Kotak Bank Sinhagad road Pune. Current account, A/C No- 2212622377
IFCS KKBK0001764
Contact for registration: Priyanka Paliwal 7507362974, Manish Ray 8149547525
Venue : GB School of neuro rehab and aquatic therapy Shop no. C5- C6, Empire Estate, old Mumbai Pune highway Chinchwad.
Upcoming workshops and lectures 2018
1. Workshop series
- MOTOR RELEARNING PART 2: Two days workshop on Advance upper limb training in stroke rehab coming soon in May 2018
- MOTOR RELEARNING PART3: Two days workshop on Advance lower limb training in stroke rehab coming soon July 2018
- Workshop “Movement dysfunction in Ataxia and its management”. 15/04/2018.
- 2 days workshop on Clinical gait analysis and management of abnormal Gait deviations. coming soon Sept 2018
- 2 days workshop on spinal cord injury rehabilitation deviations. Coming soon October 2018
- 2 days workshop on Application PNF in neuro and Musculoskelatle rehabilitation. Coming soon November 2018
2. Two to four hours Lecture series on Strategy improve motor control in stroke rehab.Dates will be announced soon
- Strategy improve motor control Trunk control
- Strategy improve motor control of Shoulder & elbow
- Strategy improve motor control of Wrist & hand
- Strategy improve motor control of hip
- Strategy improve motor control of knee
- Strategy improve motor control of ankle and foot
- Strategy improve motor control in ataxia
- Strategy improve motor control in GBS
- Strategy improve motor control in Parkinson
3. Two to four hours Lecture series on Pathomechanics and its management. Dates will be announced soon
- Pathomechanics of of Hemiplegic hand its managment
- Pathomechanics of Shoulder dysfunction in hemiplegics
- Pathomechanics of hemiplegic gait and its management
- Pathomechanics of Posture and gait in Parkinson
- Pathomechanics of ataxic gait & postural control
4. Two to four hours Lecture series on Factors affecting motor control & its management. Dates will be announced soon
- Factors affecting hyperextension of knee and its management
- Factors affecting spasticity and its management
- factors affecting motor control and motor relearning
Investment in Education about neuro rehab
To achieve this goal of my life i invested a lot in my education. I have attended multiple course by Dr. Asha Chitnis on NDT in Paediatrics.

ASha Chitnis CI NDT peads, MPT Neuro
I believe that if you want to understand neuro you need understand normal development in children and Paediatric neuro rehab. Click here for blog on this topic.
NDT Education
List of workshops i have attended for my education.
- Workshop on NDT theoretical framework & clinical applications. Dr. Asha chitins M. Sc. PT, NDT Instructor, Dr. Asha chitins M. Sc. PT, NDT Instructor. 40 Hrs. March-April 2005
- Workshop on Motor Control Problems.Asha chitins M. Sc. PT, NDT Instructor Dr. Asha chitins M. Sc. PT, NDT Instructor 40 Hrs June –July 2005
- Workshop on Rehabilitation of Adult Hemiplegia, incorporating holistic approach of Bobath, Petricia Davies Affolter concept. Dr. Roshan Vania (PT) Dr. Preeti Shah (PT). C.M.F.’s College of Physiotherapy, Nigdi, Pune. 25 Hrs 15/10/05 to 17/10/05
- Workshop on Enhancement of upper extremity function in pediatrics. Kimberley Barthel Gail Ritchi Asia-Pacific Childhood Disability Update 2005, Mumbai. Pre Conference Workshop. 17 Hrs 30/11/05 to 01/12/05
- Advance Workshop Sensory Modalities in the Treatment of Childhood Disabilities. Kimberley Barthel Asia-Pacific Childhood Disability Update 2005, BOMBAY. 8 & ½ Hrs 02/12/05 to 03/12/05
- Practice management. Sandra Moor (PT) President of world conference of physical therapy (WCPT) 43rd Annual conference of The Indian Association of Physiotherapy, at Hydrabad. 4 Hrs 22/01/05
- Neurogenic dysphasia – assessment & therapeutic management. DR.Sunita Kavrie, CCC/SLP, speech path association, inc. Indian Speech & Hearing Association, Maharashtra Branch. & Ruby Hospital, Pune. 6 Hrs. 12th December 2004
- NDT theoretical framework & clinical applications. Asha chitins M. Sc. PT, NDT Instructor Snacheti institute college of physiotherapy, shivajinagar, pune. 32Hrs October – november2005
- Motor Control, theoretical framework & clinical applications. Asha chitins M. Sc. PT, NDT Instructor Bombay 48 Hrs December2005- January 2006
- NDT Facilitation-advanced course. Asha chitins M. Sc. PT, NDT Instructor Bombay 40hrs April -June2006
- Upper limb control (NDT).Monica Diamond AWP WCPT IAP 2009 Mumbai 24hours (2Days) Jan 2009
After completing workshop with Asha Chitnis on NDT She advised me to complete your NDT certificae course. Fortunately NDT certificate course Paeds was organised in Mumbai in 2006 -2007. But i couldn’t attend that because i was going for my masters final exam. It was again organised in Pune in 2010. but unfortunately i couldn’t attend again because was busy organising the 49 Annual conference IAP Pune as joint organising secretory.
Then Asha Chitnis advised me to not do course in Paeds you do the course in Adult NDT . She helped to organise the course in 2014 in Pune.
NDT/BOBATH CERTIFICATE COURSE IN THE MANAGEMENT AND TREATMENT OF ADULTS WITH HEMIPLEGIA IN PUNE INDIA 2014
The course was suppose to start on 27th January 2014 and two Intructors Cathy Hazard (Canada) and Nicky Schmidt(USA) were suppose to arrive on early morning 26th January 2014. Both of them didn’t knew that need to get Indian VISA to arrive in India. So landed at Mumbai International Airport But got stuck in Immigaration as they were not having Indian VISA. Because of 26th January security very tight and nothing could do to help them. Our course is starting next day, all 24 participant were arrived in Pune but now the instructors couldn’t clear the immigration. Fortunatly Asha chitnis was there with me to Pick them at airport. So immigration office called me and Asha talked with the immigration officer. Asha Advised both instructors to go back get Indian Visa and come back again in few days.
 Cathy HAzzard PT CI NDT, BSc, MBA
Cathy HAzzard PT CI NDT, BSc, MBA
So both instructors gone back to their country. Cathy Hazzard from Canada got the Indian Visa Soon and she was back to India in five days. Cathy was traveling contentiously to and fro for around 6-7 days from Canada to India to Canada and again to India. unfortunately instructor from USA couldn’t get Visa in time so she didn’t return back. So ASha Chitnis assisted Cathy Hazard during the course. At last our course started five days late.
NDT workshop changed our perspective of treatment neuro rehab. Then in 2015 i have completed my advance NDT course as well.

1st Basic NDT Certificate course Batch 2014
NDTA Advanced Handling and Problem Solving Course.Cathy Hazzard, B.Sc, MBA, PT, C/NDT 01-12-2015 – 01-16-2015. A Neuro Developmental Treatment Association Approved Course. Course ID no. 15A101. Sancheti Institute College of Physiotherapy, Sancheti Health Academy Thube Park 11/12 Shivajinagar, Pune, Maharashtra, India, 41105

2nd Basic NDT Certificate course Batch 2015
I got opportunity to assist Cathy during third basic NDT course in 2016.
THIRD NDT/BOBATH CERTIFICATE COURSE IN THE MANAGEMENT AND TREATMENT OF ADULTS WITH HEMIPLEGIA, PUNE, INDIA 2016
Motor Learning Course
I was in search all the places who will teach me about different neuro rehab approaches. During search i found about course in Australia by tutors from Sydney University and Bankstown Hospital Sydney. website http://www.strokeed.com
In December 2016 i have to attend course on
Evidence-Based Upper Limb Retraining


Karl Schurr, Clinical experience in stroke and brain injury rehabilitation for 30 years+ in Australia and the UK.
This is based on work of Janeth Carr and Roberta Shepherds work (Author Motor Relearning Program). Annie and KArl also worked in stroke rehab for many years. So they formed course based on their experiences and evidences in stroke rehab. This course on upper limb and whole trip travel accommodation and food cost me around Rs 3,00,000/-
I liked their teaching and training methods so I also gone again to Australia in August 2017 for next course on
Evidence-based Lower limb Retraining

PNF courses from International PNF Association.

Karl Schurr, Clinical experience in stroke and brain injury rehabilitation for 30 years+ in Australia and the UK.
LIST OF WORKSHOP CONDUCTED BY DR. GAJANAN BHALERAO (PT)
- A) STROKE REHABILITATION WORKSHOP
- Two day Workshop on Task specific training in neuro rehabilitation, on 30 sept and 1st oct 2013, at Mission health physiotherapy center Ahmadabad, Gujarat 2013.
- Workshop “Stroke Rehab” for final year student of BPT, organized by Sancheti healthcare academy on 8/8/2015 , at Sancheti Institute College of physiotherapy.
- B) MOTOR RELARNING WORKSHOP IN STROKE REHAB
- Workshop on Motor Relearning program for stroke Rehabilitation at Youth Men Christian Association (YMCA), Pune, on 29th& 30th of March 2007.
- Workshop Motor Relearning program for stroke Rehabilitation organized by Indian Association of Physiotherapy Pune & Pimpri Chinchwad Branch on 27th &28th November 2010, at Sancheti Institute College of physiotherapy 2010.
- Workshop Motor Relearning program for stroke Rehabilitation, organized by Sancheti healthcare academy on 16th& 17th November 2014, at Sancheti Institute College of physiotherapy 2014.
- C) PROPRIOCEPTIVE NEUROMUSCULAR FACILATION WORKSHOP
- Workshop Neuro Therapeutic Approaches in Neuro Rehabilitation: Part I- Proprioceptive Neuro Muscular Facilitationorganized by Sancheti healthcare academy on 13th Sept 2014, at Sancheti Institute College of physiotherapy 2014.
- Workshop On Proprioceptive Neuro Muscular Facilitation (PNF) in Neuro Rehabilitation on 23 August and 13 September At Saifee Hospital Mumbai 2015
- Workshop Proprioceptive neuro muscular facilitation (PNF) on 23rd August and 13th September 2015 , organized by Saiffy hospital , at Saiffy hospital Mumbai.
- D) 2D & 3D GAIT ANALYSIS AND MANAGMENT
- Workshop on 2D & 3D Gait Analysis And Management Of Gait Deviations organized by Indian Association Of Physiotherapy Pune & Pimpri Chinchwad Branch on 27th & 28th November 2010, at Sancheti institute college of physiotherapy 2010.
- Workshop on 2D & 3D gait analysis and management of gait deviations organised by sancheti college of physiotherapy on 20th and 21 december 2014
- E) SPINAL CORD INJURY REHABILITAITON WORKSHOP
- Two day workshop under Indian Association of Physiotherapy Pune branch, on “Spinal Cord Injury Rehabilitation” in 2008
- Two day Workshop Spinal cord injury Rehabilitation, organized by Indian Association of Physiotherapy Pune & Pimpri Chinchwad Branch on December 2010, at Sancheti Institute College of physiotherapy 2010.
- Workshop Spinal cord injury Rehabilitation, organized by Sancheti healthcare academy on December 2012, at Sancheti Institute College of physiotherapy 2012.
- Workshop Spinal cord injury Rehabilitation on organized by Sancheti healthcare academy on August 2014 at Sancheti Institute College of physiotherapy 2014.
- Workshop “Spinal cord injury and rehabilitation” for final year student of BPT, organized by Sancheti healthcare academy on 18th and 23rd September 2015 , at Sancheti Institute College of physiotherapy.
- F) NDT/ BOABTH WORKSHOP
- Workshop on NDT/ Bobath approach workshop for 3rd Year BPTh on August 2015 Workshop “Neuro developmental therapy (NDT)/Bobath” for third year student of BPT, organized by Sancheti healthcare academy on 22/8/2015 , at Sancheti Institute College of physiotherapy.
List of workshop attended by DR. Gajanan Bhalerao (PT)
Neuro Rehab workshop
- Workshop on NDT theoretical framework & clinical applications. Dr. Asha chitins M. Sc. PT, NDT Instructor, Dr. Asha chitins M. Sc. PT, NDT Instructor. 40 Hrs. March-April 2005
- Workshop on Motor Control Problems.Asha chitins M. Sc. PT, NDT Instructor Dr. Asha chitins M. Sc. PT, NDT Instructor 40 Hrs June –July 2005
- Workshop on Rehabilitation of Adult Hemiplegia, incorporating holistic approach of Bobath, Petricia Davies Affolter concept. Dr. Roshan Vania (PT) Dr. Preeti Shah (PT). C.M.F.’s College of Physiotherapy, Nigdi, Pune. 25 Hrs 15/10/05 to 17/10/05
- Workshop on Enhancement of upper extremity function in pediatrics. Kimberley Barthel Gail Ritchi Asia-Pacific Childhood Disability Update 2005, Mumbai. Pre Conference Workshop. 17 Hrs 30/11/05 to 01/12/05
- Advance Workshop Sensory Modalities in the Treatment of Childhood Disabilities. Kimberley Barthel Asia-Pacific Childhood Disability Update 2005, BOMBAY. 8 & ½ Hrs 02/12/05 to 03/12/05
- Practice management. Sandra Moor (PT) President of world conference of physical therapy (WCPT) 43rd Annual conference of The Indian Association of Physiotherapy, at Hydrabad. 4 Hrs 22/01/05
- Neurogenic dysphasia – assessment & therapeutic management. DR.Sunita Kavrie, CCC/SLP, speech path association, inc. Indian Speech & Hearing Association, Maharashtra Branch. & Ruby Hospital, Pune. 6 Hrs. 12th December 2004
- NDT theoretical framework & clinical applications. Asha chitins M. Sc. PT, NDT Instructor Snacheti institute college of physiotherapy, shivajinagar, pune. 32Hrs October – november2005
- Motor Control, theoretical framework & clinical applications. Asha chitins M. Sc. PT, NDT Instructor Bombay 48 Hrs December2005- January 2006
- NDT Facilitation-advanced course. Asha chitins M. Sc. PT, NDT Instructor Bombay 40hrs April -June2006
- Upper limb control (NDT).Monica Diamond AWP WCPT IAP 2009 Mumbai 24hours (2Days) Jan 2009
- NDT/Bobath certificate course in the management and treatment of adults with hemiplegia and head injury. Cathy Hazzard, B.Sc, MBA, PT,C/NDT19 January –06 February 2015. A Neuro Developmental Treatment Association Approved Course.Course ID no. 14A101. Sancheti Institute College of Physiotherapy, Sancheti Health Academy Thube Park 11/12 Shivajinagar, Pune, Maharashtra, India, 41105
- NDTA Advanced Handling and Problem Solving Course.Cathy Hazzard, B.Sc, MBA, PT, C/NDT 01-12-2015 – 01-16-2015. A Neuro Developmental Treatment Association Approved Course. Course ID no. 15A101. Sancheti Institute College of Physiotherapy, Sancheti Health Academy Thube Park 11/12 Shivajinagar, Pune, Maharashtra, India, 41105
- Motor Relearning : evidence based upper extremity training. At Bankstown Limbcobe hospital , Sydney Australia December 2016.
- Motor Relearning : evidence based lower extremity training. At Bankstown Limbcobe hospital , Sydney Australia August 2017.
Gait Analysis
- Three days 2D and 3D gait analysis workshop by Dr. Abhay Khote (Consultant Orthopaedic Surgeon at The Royal Children’s Hospital Australia) and Jill Rodha (Physiotherapist Australia) from Hugh Williamson Gait Analysis Laboratory gait lab team organised by Rehab department of Kokilaben Ambani hospital at 3D Gait lab of Kokilaben Ambani hospital Mumbai in 2011.
Research workshops
- Seven days advacne work on rsearch methodalogy for Pre Phd training.16thApril to 22nd April 2014, organised by MUHS Nashik at MUHS nashik.
- Workshop on Manuscript writing for publication at YASHADA Baner, PUNE, Jan 2013
- Research methodology workshop by MUHS Nashik at Regional centre Medical education technology (MET) cell Pune 2012.
- Clinical Research & Research methodology workshop by Dr. Mohit Bhandari (Canada Research Chair in Musculoskeletal Trauma) , organised by Sancheti Hospital at Sancheti hospital 2008
- Research methodology workshop by Dr. Dhara Kapoor Nuero therapist USA, organised by TEAM physiotherapy centre Pune at Band garden Hotel Pune l 2010
- Workshop on Grant writing for Research organised MUHS Nashik at Regional centre Medical education technology (MET) cell Pune at Sancheti Hospital at Sancheti hospital 2013
Medical Education
- Three days Basicworkshop on Medical education technology by Maharashtra university of health sciences MUHS Nashik at Regional center Medical education technology (MET) cell Pune 2012.
- Seven days advance workshop on Medical education technology by Maharashtra university of health sciences MUHS Nashik at Regional center Medical education technology (MET) cell Pune 2013.
Social Media and Networking
- Workshop of social media and networking organised by Sancheti healthcare academy. This workshop was training of how to use social media and blog.
Dance
- I am trained in Salsa dance by Rocky Poonawala dance academy Pune








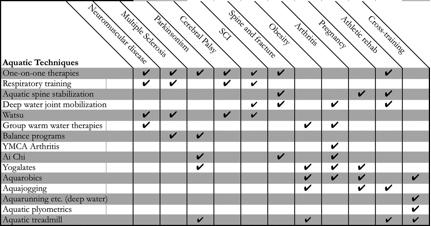













































































































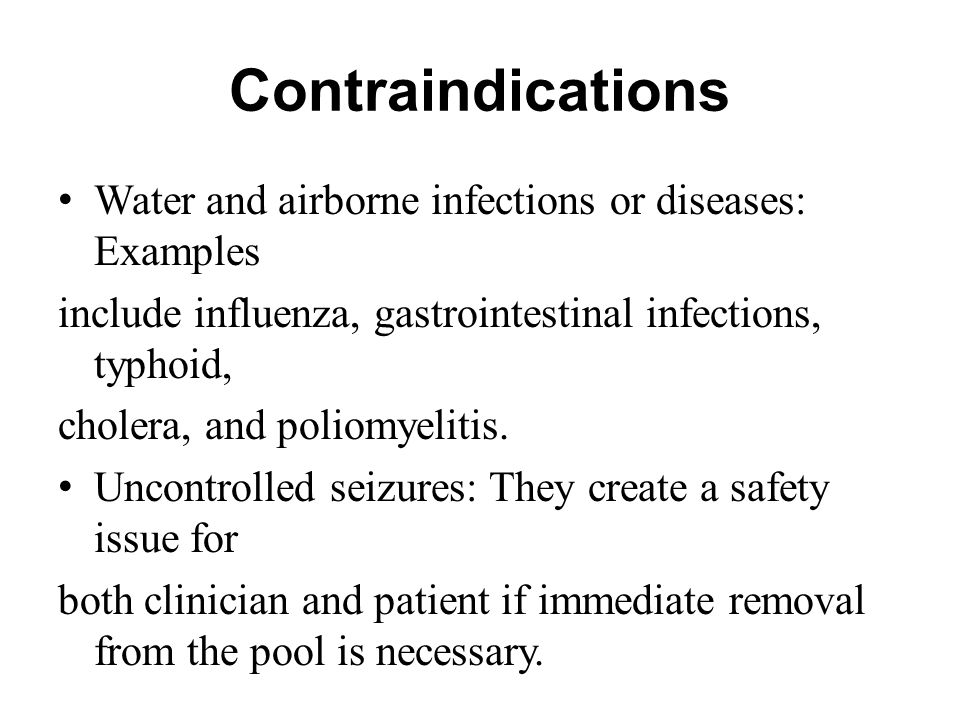 Frequently Asked questions about Aquatic therapy ?
Frequently Asked questions about Aquatic therapy ?



















































You must be logged in to post a comment.